How to Overcome Contact Tracing Challenges in Senior Living Facilities

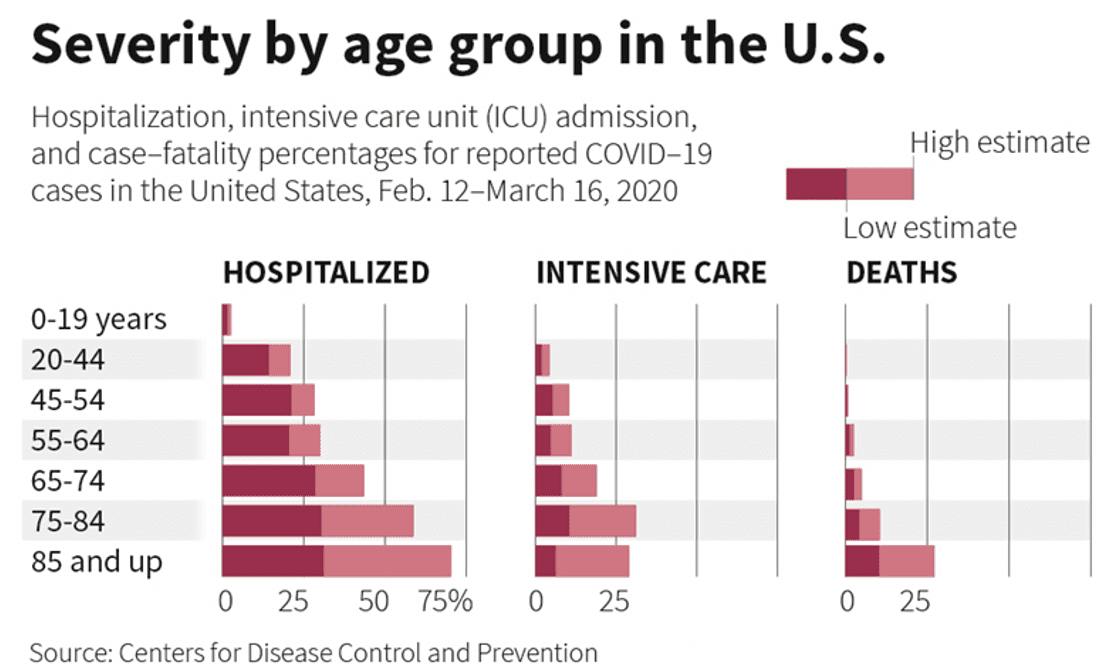
Older adults, particularly those with underlying health conditions, are at a higher risk for severe COVID-19 associated illness and death. According to the CDC, 8 out of 10 coronavirus-related deaths reported in the US have been in adults 65 years and older. Federal government figures released earlier this week, reveals more than 400 senior living and nursing facilities in the United States have at least one resident who has tested positive for coronavirus. With these facilities fast becoming the hot spot for the spread of the virus, there has been a particular emphasis on infection control and measures to curtail the spread of COVID-19. Successful coronavirus responses from China, Singapore, Hong Kong, and South Korea outline three crucial steps – Rapid Testing, Contact Tracing, and Quarantine.
CDC’s criteria for uation and laboratory testing for COVID-19 has placed identifying and triaging those who are at the highest risk of infection as Priority #2. These include patients in long-term care facilities such as nursing homes and senior living communities and patients 65 years or older with symptoms. However, it is worthwhile to note that this omits the population that may be carrying the virus without showing any symptoms. Estimates of covert cases suggest that they could represent 60% of all infections, and recent reports by the CDC on residents in a nursing home indicate that 57% of residents that tested positive for COVID-19 were asymptomatic or presymptomatic on the day of testing. This finding is significant because it suggests several things: 1. Symptom-based screening of residents may fail to identify individuals (residents, visitors and staff) that are infected with COVID-19; 2. Transmission from asymptomatic or presymptomatic residents, visitors and staff, who were not recognized as having COVID-19 infection and were therefore not isolated, might contribute to further spread in a community.
Once those infected or showing typical COVID-19 symptoms (fever, cough, and shortness of breath) have been identified, comes the most significant challenge and crucial step in effectively stopping the spread of the virus — Contact Tracing.
What is Contact Tracing?
Contact Tracing is a public health response that entails retracing the recent movements of a person who has tested positive for COVID-19 and to find, test, and isolate anyone who has come in contact with the person. Germany, South Korea, and Singapore have deployed aggressive contact tracing to curtail the spread of coronavirus. These range from issuing media advisories, using security camera footage, to tracking suspected carriers with police investigations.
How is Contact Tracing done?
Historically, Contact Tracing is conducted by interviewing an infected person, learning about their movements, and identifying all close contacts. The shortcoming of such a process is that it relies on anecdotes, faulty memory recall and cannot reliably find all the contacts an infected individual had. Given that COVID-19 can have an incubation period of up to 2 weeks, an infected individual may have to recall up to two weeks of movements and contacts.
Why is Contact Tracing hard to do in nursing homes and senior living communities?
The challenge is exacerbated in nursing homes and senior living communities as they house a population highly vulnerable to the virus, living in close quarters to each other. Time is of the essence in backtracking an infected individual or a person showing symptoms and taking necessary measures to isolate or test everyone who has been exposed to that person. Apart from residents and staff, senior living facilities receive visitors, contractors, visiting nurses, and a host of other foot traffic. Understanding everyone a person may have come in contact with, ranging to a timeframe that could span days up to two weeks, is a herculean task. Further, relying on effectively tracing through recollection from seniors who are commonly known to have memory issues, adds another layer of complexity to contact tracing in nursing homes and senior living communities.
How can technology help?
Technology can play a vital role in expediting this process and accurately pinpointing where the person has been and who they have come in contact with. Singapore launched a contact-tracing smartphone app to allow authorities to identify those who have been exposed to people infected with coronavirus as part of efforts to curb the spread of the disease. MIT researchers recently announced the launch of a project that tracks COVID-19 patients through mobile phones. When it comes to Contact Tracing an infected individual, operators of nursing homes and senior living facilities must look at three factors:
Who the infected individual came in contact with?
Where did the infected individual visit within the facility?
Who was in the same room as the infected individual?
CarePredict recently announced CarePredict PinPoint — a toolset that helps nursing homes and senior living facilities stop the spread of coronavirus by automating contact tracing.
CarePredict Contact Tracing report
Who they came in contact with?
CarePredict uses its real-time indoor location technology in its PinPoint Contact tracing tool to quickly retrace the path of an infected individual, understand who they have come in contact with, and the duration for which they have been exposed. The automated tracing process can be completed with the push of a button instead of an arduous process of interviewing each individual and most importantly, doesn’t rely on recall by memory.
Where has the person been?
When a person is showing symptoms or has been tested positive, facilities need to quickly sanitize and disinfect all of the areas the person has visited. Tools like CarePredict’s PinPoint Path Tracing tool provides immediate visibility into the areas visited by the carrier so that staff can use enhanced disinfection protocols in these areas.
Who was in the same room as the infected individual?
Epidemiologists or “disease detectives” in Connecticut were busy tracking down over 400 people who were present at a funeral service that was attended by a man recently tested positive for COVID-19. Understanding who was in the same place at the same time as, or shortly after, an infected individual helps identify people who must be tested quickly as the coronavirus can linger in the air or on surfaces from minutes to potentially hours. CarePredict’s PinPoint Room Traffic tool presents a detailed list of all people who were in the rooms visited by an infected individual along with timestamp and duration.
Replay Map:
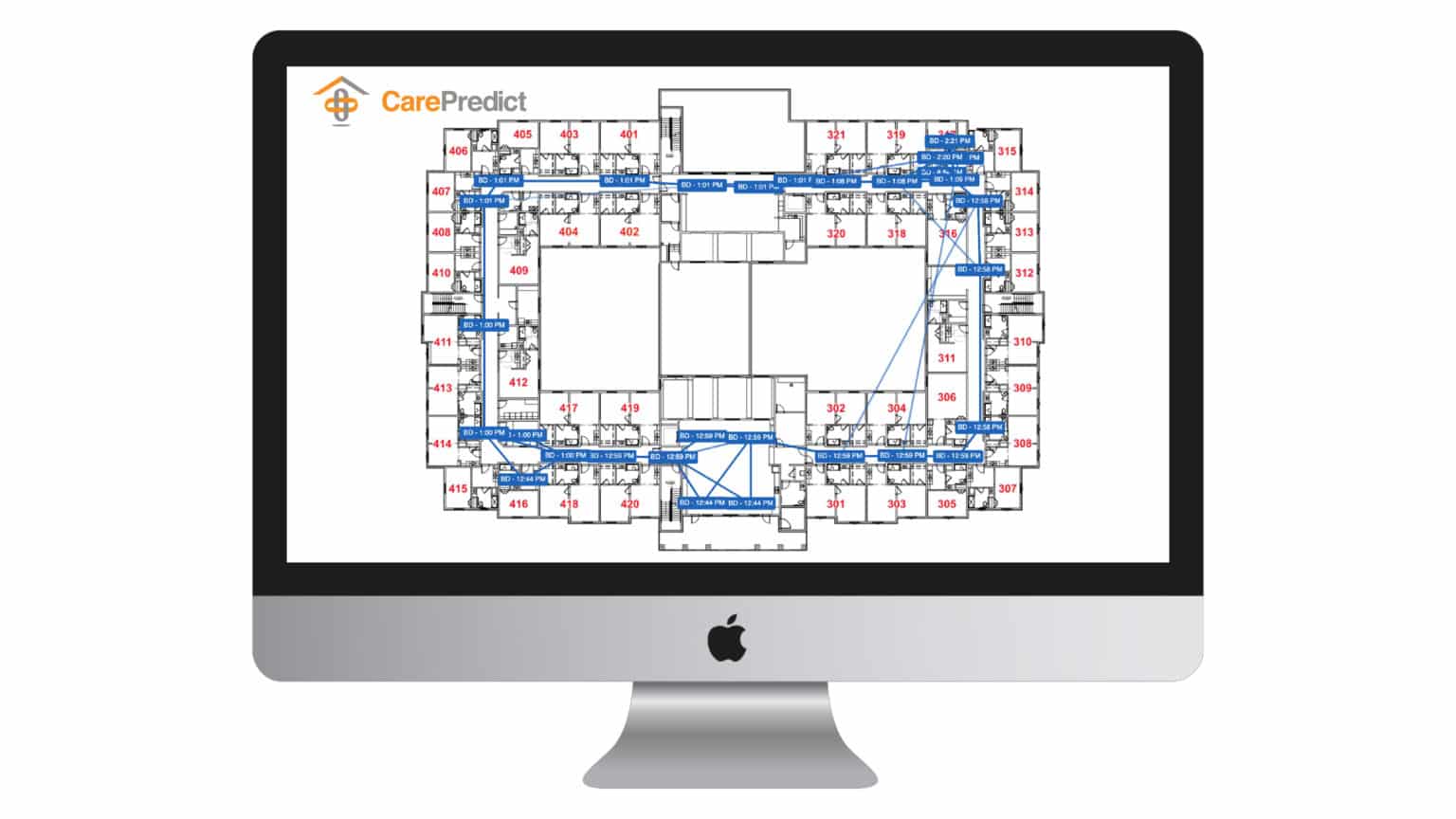
Last but not least, CarePredict PinPoint Path Tracing tool provides a one-glance view of the path an infected person took through a facility in a specific period.


Related Blogs






