.avif)
Predict Health Declines
Prevent Hospitalizations
Protect Your Residents
CarePredict is the Resident Care Platform built exclusively for the most innovative senior living operators.
our impact
Real Results. Measurable Impact. Proven Platform.
$320k+
Captured in unbilled care services at Edgewood Healthcare
39%
Lower hospitalizations at Lifewell Senior Living
60%
Improved UTI recovery times by detecting them earlier at Bickford
37%
Increase in staff efficiency at Paradise Pointe
67%
Increase in length of stay from National Institute of Health Study
13
Years serving the senior living indusry
THE RESIDENT CARE PLATFORM
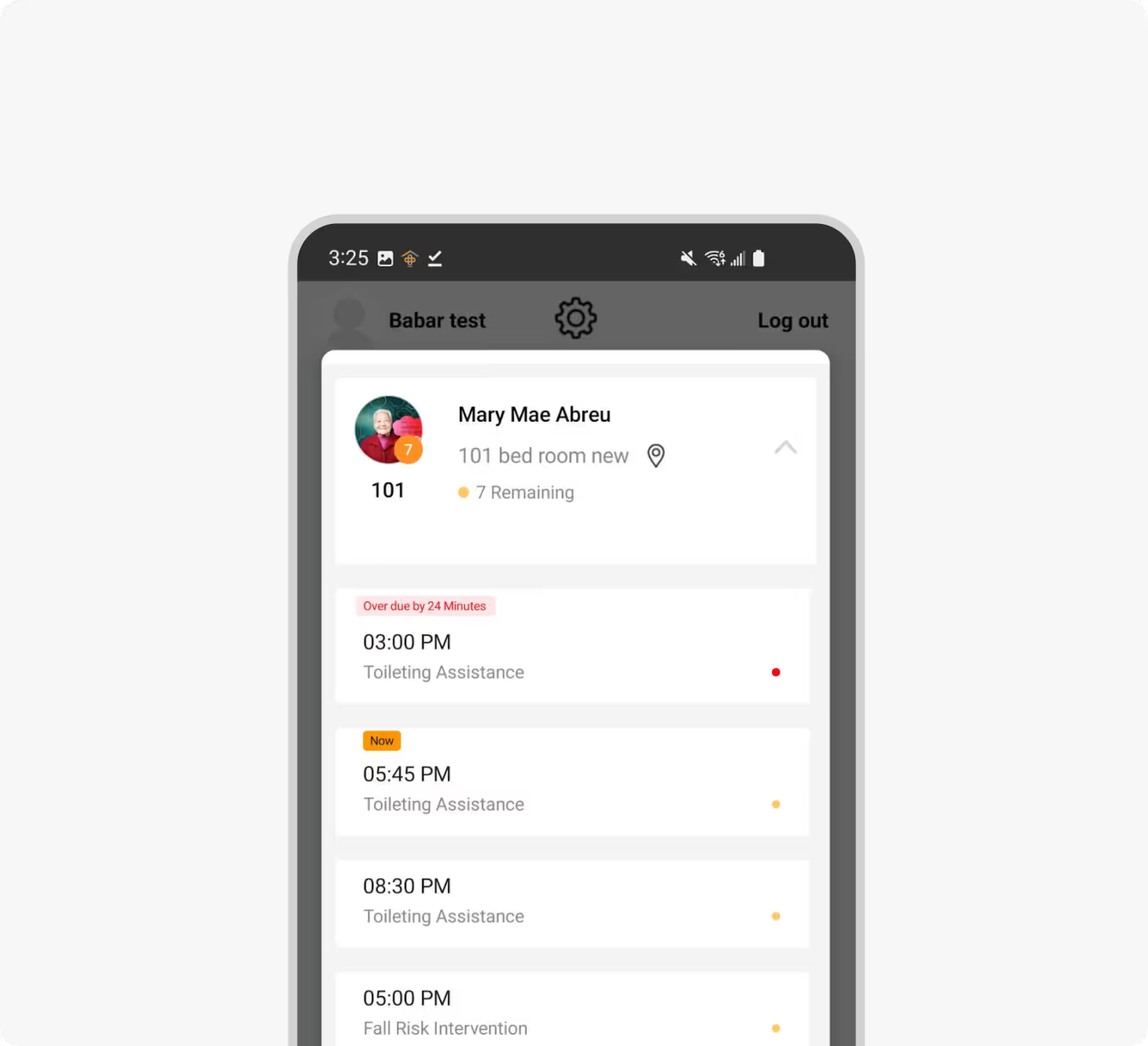
One Platform. Better Care. Happier Teams.
Award Winning Solution. Proven in Senior Living.
Testimonials
What People are Saying About CarePredict
Our Clients
Who We Serve

Independent Living
Proactive care without being intrusive—residents live freely, safely, and families stay informed.


Memory Care
Protect your most vulnerable residents with real-time location insights, elopement prevention, and predictive alerts.

Assisted Living
Balance quality care with operational efficiency. Reduce staff overload while improving resident satisfaction.

Residential Assisted Living Communities
Bring enterprise-grade care technology to your smaller homes with affordable, scalable solutions.